Symptoms and Etiology of Servere and Persistent Mental Illness
The most common diagnoses of individual who participate in rehabilitation programs are Schizophrenia and Mood Disorders.
Why is it that these would be the most common?
The symptoms of these disorders have physiological, psychological, and social consequences. The disabling nature of these disorders is that they can be severe and persistant.
Symptoms
The symptoms of a mental illness involve the persons senses, emotions, and cognition.
Persistence
This term refers to the point that many of the symptoms are “long lasting”. This presents a special challenge to psychiatric rehabilitation, as we are not so much in the business of helping individuals overcome their symptoms but to learn to live with them.
SCHIZOPHRENIA
The DSM classifies the symptoms of S. into two broad categories, negative (diminution or loss of normal functions) and positive (an excess or distortion of normal functions) symptoms.
Positive Symptoms
- Thinking and ideas (delusional)
- Perceptions and sensations (hallucinations and illusions)
- Language and communication (disorganized or bizarre speech)
- Behavior self-control (grossly disorganized or catatonic behavior)
Negative Symptoms
- The range and intensity of emotional expression (flat affect)
- The fluency and productivity of thought and speech (alogia)
- The initiation of goal-directed behavior (avolition)
How would each of these impact the individuals physiological, psychological, and social functioning?
When we encounter people with these symptoms what assumptions do we make about them (not knowing that they have a mental illness)?
Delusions
Delusions include bizarre beliefs or ideas that the person cannot be talked out of. A common one is that one’s actions may be under the control of others. Others include grandiose ideas of the self. (These might include ideas of being famous, being close to famous individuals/God, or being targeted by others such as the FBI and/or Secret Service)
Delusions (and hallucinations) are “real” to the person…they will act in accordance to these belief systems as much as you and I react to any belief system we have.
Hallucinations
Hallucinations involve sensory stimulation or information that the person experiences as real. The most common are auditory in nature (hearing voices/instructions, command hallucinations---it is no surprise that we thought that individuals with Schizophrenia were possessed by demons!)
Thought Disorder
Disordered thoughts in a person with schizophrenia might include thought broadcasting, confusion, thought insertion, and racing thoughts.
The experience of Symptoms…
It is difficult for us to know how individuals really experience their symptoms. Do they hear a disembodied voice or is it something like self-talk? Different individuals react differently to these symptoms as well. But for the individual, these are very real.
Some individuals learn to live along with their symptoms by learning to manage their behaviors despite the symptomology.
Phases of Schizophrenia
- Prodromal
- Suspicious that SOMETHING is going on, withdrawal from social contacts, etc.
- Acute
- Full-blown symptoms
- Residual
- Symptoms are milder or perhaps more adapted to
How would going through these phases impact the physical, psychological, and social aspects of someone’s life?
MOOD DISORDERS
Mood disorders impact a smaller number of individuals who are in psychiatric rehabilitation centers. Some symptoms are mild to moderate while others can be quite severe. Individuals sometimes “cycle” between periods of relatively normal functioning and dysfunction.
Symptoms
- Depressive episode (may end up with a diagnosis of Major Depression)
- Manic episode
- Mixed episode (may end up with a diagnosis of Bipolar Disorder)
Depressive Episode
- Depressed mood most of the day
- Markedly diminished interest or pleasure in all, or almost all, activities
- Significant weight loss when not dieting or weight gain (appetite)
- Insomnia or hypersomnia
- Psychomotor agitation
- Fatigue or loss of energy
- Feelings of worthlessness or excessive inappropriate guilt
- Diminished ability to think or concentrate
- Recurrent thoughts of death, suicidal ideation/plans/attempts
Manic Episode
- Inflated self-esteem
- Decreased need for sleep
- More talkative than usual
- Pressured speech
- Flight of ideas
- Distractibility
- Increased goal directed activity
- Excessive involvement in pleasurable activities that have a high potential for painful consequences
The RISK of Diagnosis
It is rare that a person’s symptoms fall neatly into categories such as this. Diagnosing is as much an art as it is a science. This means that diagnosing needs to be somewhat flexible and we need to understand that categories can rarely capture the specific nature of what it is a person is dealing with. Diagnosis drives the use of medications so it is very important to get the right diagnosis and change it if the medication is not effective.
Dual Diagnosis
Dual diagnosis refers to the presence of two coexisting conditions
- Mental Illness and Developmental Disabilities
- Mental Illness and Substance Abuse
The Role of PsyR
It is important to remember that most psychiatric rehabilitation interventions are not designed to address symptoms, but to address the impairments and barriers that result from the symptoms. The focus of PsyR is on the strengths and abilities that the person has which will allow them to live with the symptoms.
Too much emphasis on diagnoses and symptoms may lead the practitioner down the wrong road for treatment (since diagnosing can be problematic)
ETIOLOGY OF MENTAL ILLNESS
So where does this all come from? In the history books of psychology the assumption was that mental illness arose from internal conflicts and anxiety (psychodynamic approach).
New technology is pointing toward a much more biological source of the trouble. Biological issues that may be related to mental illness include:
Physiological Structure in the Brain
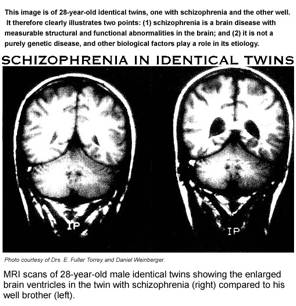
MRI (Magnetic Resonance Imaging) scans identify differences in the physiological structures of the brain. Persons with schizophrenia tend to have larger ventricles in their brains.
PET (Positron Emission Tomography) scans provide a colored picture of the brains blood flow and process of metabolizing glucose. Studies have shown that parts of the brain (namely the Frontal Lobe) are less active in individuals with schizophrenia.
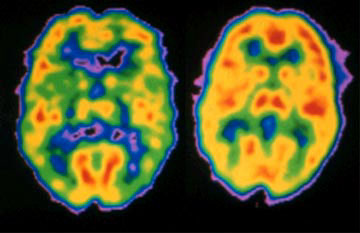
Color in the image above indicates more activity…the brain on the right is a normal brain, the brain on the left is one from a person with schizophrenia
Neurotransmitters and Mental Illness
Neurotransmitters are the communication chemicals in the brain. They ensure proper functioning and operations within the brain.
Some of the major neurotransmitters are:
- Dopamine (involved in all sorts of behavior including movement, hearing, and planning)
- Norepinephrine (also known as adrenaline, is involved with the circulatory system, the heart, but also affects sleep, appetite, and sexual behavior)
- Serotonin (affects sleep, impulse control, and other functions)
- Acetylcholine (movement and muscles)
Dopamine and Serotonin seem to be involved in schizophrenia
Serotonin and Acetylcholine seem to be involved with mood disorders
Many medications that are provided for individuals with mental illness impact the neurochemistry of the brain in an effort to control symptoms.

Resources
In this field the definitive guide to diagnosing is the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-IV-TR)
Although there are other sources for information about diagnoses, this is the ONLY source you should turn to to get diagnostic criteria for academic and clinical work.
Links
This is a great site sponsored by the National Institute of Health
http://science-education.nih.gov/supplements/nih5/Mental/guide/info-mental-a.htm