Lesson 9: Confrontation
Attention

Sometimes we don't agree with the person we are interviewing or counseling. While we have nurtured a sense of multicultural awareness and alternative points of view, we might still want to "change someone's mind" about something when they are seeing things from a particular point of view or their thoughts are irrational.
Picking how and when to do this are key questions for the counselor. It is somewhat of a test of how good a relationship you have developed up until now!
Learning Outcomes
Upon completion of this lesson's material, students will be able to:
- Identify personal "problem solving" and "conflict avoiding" styles of interaction
- Reflect on the role that your personal style may play in your own efforts to confront your clients
- Reflect on personal stories regarding your own experiences with confrontation
- Understands role of medication in symptom management (MHRT/C Outcome)
Teaching
Confrontation
Confrontation is one of the most difficult skills for the same reason it is hard to reflect feeling...we are not used to dealing with feelings and many of nurture a pretty good habit of AVOIDING conflict. In confrontation, you are taking the risk that conflict might arise.
Styles of Confrontation
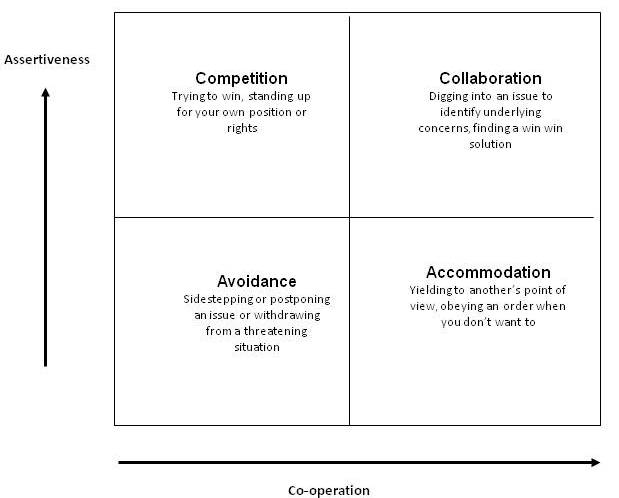
The most widely understood model for Styles of Confrontation is the Thomas-Killman model.
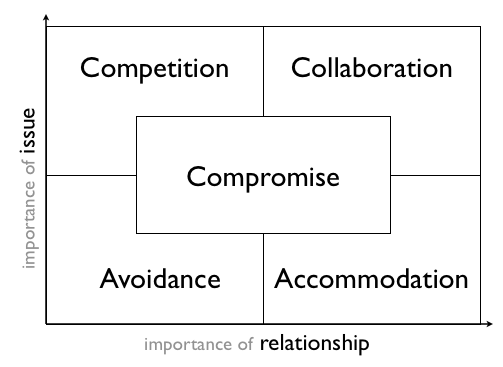
This particular model focuses on the dimensions of the "importance of the issue" and the "importance of the relationship" This next graphic represents the basic styles of each of the four quadrants..."Compromising Style" is a combination of all of them.
Another model to assist us in understanding our own style is the Myers-Briggs Typology.
Click here to download an Excel file which contains a shortened version of the Myers-Briggs Typology test. To assist in your personal interpretation of your Myers-Briggs Typology Test...visit TypeLogic But, yes...there is an app for this...the Jungian Type Questionnaire!
This app simply provides a way to take the test, get your letter combination and then some additional information on the interpretation of the results. There are literally thousands of websites on how to use these scores. Five Tips for using the Using the MBTI in Conflict Using the Myers-Briggs Type Indicator to Enhance Workplace Communication |
Opportunities for Confrontation in the Counseling and Interviewing Process
- Immobility
- Blocks
- Repetitive compulsions
- Inability to achieve goals
- Lack of understanding
- Limited behavioral repertoire
- Limited life script
- Impasse
- Lack of motivation
Steps in Confrontation
- Identify the conflict...(call it what it is)
- Point out the issue
- Evaluate the change
Medications and Mental Health
One of the more common issues that comes up with many of our clients centers around their relationship with the psychotropic medications that they take.
While compliance with doctors' orders is a problem across all populations, it is particularly serious among this population. A client who really "needs" to be on his meds can get into a lot of trouble when they are not on them. This is not only a personal/rehabilitative/medical issue, but a public issue as well.
Review the following articles and consider how we ensure good Psychosocial practice while concurrently keeping the public safe.
Hospitalization, Medication Key Factors in Treating Mental Illness With a critical exception, mentally-ill people are no more likely than anyone else to commit violent crimes, according to mental health professionals. A drastic difference comes into play, however, when patients are released from hospital stays that are shorter than in the past. They can refuse outpatient treatment. And even those willing to take medication and/or counseling might not find it in a fragmented system, experts say. William Bruce, who has been charged with murder in the death of his mother, Amy Bruce, had been diagnosed with schizophrenia, and was in and out of hospitals, according to his father's report to police. Amy Bruce's body was found Tuesday by her husband, Robert, who told police that he found her body in the bathtub of their Caratunk home and it appeared that her throat was cut. In a police affidavit filed in Portland District Court, Maine State Police Detective Jeffrey Love said Bruce told him "that his son suffered from mental illness and had spent three months in Riverview (Psychiatric Center in Augusta). Since being home from Riverview, William refused to take his medication and his behavior was 'out of control.' " Police caught up with William Bruce, 25, in South Portland. He had articles belonging to his mother with him, according to Love's affidavit. Riverview Superintendent David S. Proffitt said Wednesday finds that the mental-health system is lacking following a patient's discharge. "In Maine, a client can choose not to be engaged in treatment, and the level of dangerousness rises," Proffitt said. "The major issue is when someone does not appear eminently dangerous and cannot be committed." William Bruce, according to his father's report to police, had been angry of late. Proffitt said it is not unusual for a paranoid schizophrenic to believe his next-door neighbor wants to kill him. "Major thought disorders like schizophrenia, especially when it involves delusions of persecution and command hallucinations, are more apt to violence," Proffitt said. "It's generally done for self-preservation." In 1996, Mark Bechard, a mental patient who had not been taking his medication, went on a rampage at Waterville's Servants of the Blessed Sacrament convent, killing two nuns and injuring two others. Mark Bechard visited the chapel regularly, and knew the nuns he stabbed and bludgeoned. Bechard also suffers from a schizoaffective disorder and was in the midst of a psychotic episode when he went on the rampage. Bechard was found not guilty by reason of insanity following a trial. He was committed to the custody of the state mental hospital in Augusta. Following years of medical and social supervision, psychiatrists and psychologists there said his behavior has been exemplary. In April, a judge granted Bechard the freedom of unsupervised activities at structured events within a 10-mile radius of Augusta. Bechard must be supervised in a church, and his workplace must be outside of Winslow, Waterville, Fairfield and Oakland. Both William Bruce and Bechard were living unsupervised lives as the result of a 1990 consent decree between lawyers representing patients at the former Augusta Mental Health Institute (AMHI) and the state. In the 1970s and on into the 1980s, there was a cry for change. Health-care professionals, sociologists and politicians had concluded that patients in mental institutions were living under inhumane conditions and the campaign for change began. In essence, the decree was intended to decrease the number of patients at the Augusta Mental Health Institute, and turn those patients over to an improved community health system. Sixteen years later, mental health professionals in Maine give the state's community care system a decent grade. But integration of services is a major concern, they say. Proffitt said Maine has a rich array of community mental health services. Better continuity from one service to another, however, is a priority, he said. Helen Bailey, a plaintiffs' lawyer at the Disability Rights Center in Augusta, was involved in the landmark court decision that essentially deinstitutionalized mental health care. Integration, distribution and flexibility of services is a concern, she said. "Most of the basic components are all there," Bailey said. "I do have some concerns about crisis service. Crisis resolution people must be involved with clients as much as possible." Community providers, Bailey said, do not participate in the decision to discharge patients from a hospital. Not allowed to bill Medicaid, they are not allowed to practice when their clients are in the hospital. The client goes back to the community, and the provider is not familiar with new medications or treatment. "The hospital can make a recommendation for discharge on the basis of a stay in the hospital," Bailey said. "That's not the person who's living in the real world. Judging what you need on the outside based on what you see on the inside can be a limited view." Simonne Maline, peer services coordinator for Amistad, said there are deficiencies in the community system. Amistad provides peer support for those with mental illness at its recovery center in Portland. "It's not properly funded, but it's getting there," Maline said. "There are lots of holes in the community system, especially with hospitalization. Hospitalizations can be very short." Maline also said that people with mental illnesses are more likely to be victims than perpetrators, and if they stay on their programs, no more likely than anyone else to commit crimes. "You don't hear about the people who are doing great things with their lives," she said. Once a patient undergoes a quick medical analysis, Maline said, he or she is out of the hospital. And there is less outreach for that patient now because the services are not always billable. "The system is fragmented because agencies need money to survive," Maline said. "Now, to get services, a person must have MaineCare or a diagnosis to trigger a funding system." Maline also pointed out that there are far fewer psychiatrists in rural areas such as Caratunk. Larry Grard -- 474-9534, Ext. 343 lgrard@centralmaine.com Copyright Morning Sentinel Jun 23, 2006 Nun's Killer out of Riverview (update) |
Assessment
Lesson 9 Quiz
- Discuss your thoughts about how you might approach the use of medications in psychiatric treatment. Consider that you will be dealing with a number of clients who would prefer that they didn't have to take the medications they are taking. How can we be psychosocial and still convince people to do what is best for them?
Lesson 9 Discussion
I would like you to review the conflict resolution models (and the Myers-Briggs test if you can complete that one as well) and find how you personally deal with conflict. Conflict in the counseling process can be emotional and thus we might avoid it the same we discussed how we avoid feelings (in the previous lesson). Discuss how do you feel that your confrontation/conflict resolution style may positively and/or negatively impact your work with clients.

