Lesson 7: Bio-Medical Perspective
Attention

Let’s start with some laughs, because this lesson is mostly stats and may be difficult
Learning Outcomes
Upon completion of this lesson's material, students will be able
- Examine ideas related to dying and death in health care settings, end-of-life ethics, dying as it relates to terminal or life-threatening illness and the concepts of grief and loss related.
- Assess health care practices based on an understanding of the biological and social factors that contribute to definitions of death/life.
- Articulate one or more definitions, theories, or models that describe health-care and death-care.
Teaching
Read Chapters 5 & 8 in course text.
Chapter 1: Establishing the Perspective
And the New York Time’s brief report regarding Terri Schiavo.
The overriding themes of this lesson are the medical definitions and statistical information regarding death and dying. Biological, anatomical, physiological and underlying mechanisms of health and disease will be explored. Students will explore these concepts by examining “health” and the functions of a healthy human; and, “death” / “dying” and the functional issues involved in these processes. What do these terms mean, in medical terms? Or, social terms? The functions of a healthy human suggest an understanding of the underlying mechanisms of life and death, health and disease.
Read this article regarding The Ethics of Ending Life: Euthanasia and Assisted Suicide
The Center for Disease control and Prevention compiled data in a report spanning 75 years in the United States, 1935-2010. Key findings of the 75 Years of Mortality in the United States are as follows:
- Although single year improvements in mortality were often small, the age-adjusted risk of dying dropped 60 percent from 1935 to 2010.
- Heart disease, cancer, and stroke were among the five leading causes every year between 1935 and 2010.
- The risk of dying decreased for all age groups but was greater for younger age groups with a 94 percent reduction in death rates at 1–4 years compared with a 38 percent decline at 85 years or more.
- Age-adjusted death rates were consistently greater for males than females (for example, 65 percent higher than those for females between 1975 and 1981 compared with 40 percent higher in 2010) as each decreased substantially between 1935 and 2010.
- The risk of dying decreased for all race subgroups of the U.S. population from 1935 to 2010; however, differences persisted between groups (the gap was the widest between 1988 and 1996).
What explanations can you offer for these differences? What was happening in the United States during this time period? What was changing? Use the bio-psycho-social model to better understand the interconnectedness of these improvements and/or changes. Reductions in deaths and death rates are often used as an indicator of the success of public health initiatives to improve the health and well-being of the U.S. population, as well as to set national goals for reducing disparities in the burden of mortality across groups. Anti-tobacco campaigns, AIDS prevention programs, and cancer screening promotions all use lives saved as a measure of success. What other historic phenomenon was occurring during this time period? What about wars, epidemics, cultural upheavals, counter-culture movements and improvements in technology?
Death
From: http://medical-dictionary.thefreedictionary.com/Death
Definition
Death is defined as the cessation of all vital functions of the body including the heartbeat, brain activity (including the brain stem), and breathing.
Description
Death comes in many forms, whether it be expected after a diagnosis of terminal illness or an unexpected accident or medical condition.
Terminal illness
When a terminal illness is diagnosed, a person, family, friends, and physicians are all able to prepare for the impending death. A terminally ill individual goes through several levels of emotional acceptance while in the process of dying. First, there is denial and isolation. This is followed by anger and resentment. Thirdly, a person tries to escape the inevitable. With the realization that death is eminent, most people suffer from depression. Lastly, the reality of death is realized and accepted.
Causes and symptoms
The two leading causes of death for both men and women in the United States are heart disease and cancer. Accidental death was a distant third followed by such problems as stroke, chronic lung disorders, pneumonia, suicide, cirrhosis, diabetes mellitus, and murder. The order of these causes of death varies among persons of different age, ethnicity, and gender.
Diagnosis
In an age of organ transplantation, identifying the moment of death may now involve another life. It thereby takes on supreme legal importance. It is largely due to the need for transplant organs that death has been so precisely defined.
The official signs of death include the following:
- no pupil reaction to light
- no response of the eyes to caloric (warm or cold) stimulation
- no jaw reflex (the jaw will react like the knee if hit with a reflex hammer)
- no gag reflex (touching the back of the throat induces vomiting)
- no response to pain
- no breathing
- a body temperature above 86 °F (30 °C), which eliminates the possibility of resuscitation following cold-water drowning
- no other cause for the above, such as a head injury
- no drugs present in the body that could cause apparent death
- all of the above for 12 hours
- all of the above for six hours and a flat-line electroencephalogram (brain wave study)
- no blood circulating to the brain, as demonstrated by angiography
Current ability to resuscitate people who have "died" has produced some remarkable stories. Drowning in cold water (under 50 °F/10 °C) so effectively slows metabolism that some persons have been revived after a half hour under water.
What is life? What is death? When do we pass from one to another, and can we move back and forth? Who decides when someone is alive? Dead? What are some factors in evaluating ‘treatment’?
A valuable resources to explore is:
http://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
This document contains the Detailed Tables for the National Vital Statistics Report (NVSR) “Deaths: Final Data for 2013.”
Death in the United States
- Death rate: 821.5 deaths per 100,000 population
- Life expectancy: 78.8 years
- Infant Mortality rate: 5.96 deaths per 1,000 live births
Number of deaths for leading causes of death:
- Heart disease: 611,105
- Cancer: 584,881
- Chronic lower respiratory diseases: 149,205
- Accidents (unintentional injuries): 130,557
- Stroke (cerebrovascular diseases): 128,978
- Alzheimer's disease: 84,767
- Diabetes: 75,578
- Influenza and Pneumonia: 56,979
- Nephritis, nephrotic syndrome, and nephrosis: 47,112
- Intentional self-harm (suicide): 41,149
Source: Deaths: Final Data for 2013, tables 1, 7, 10, 20
The CDC Wonder interactive tool to explore the underlying cause of death of groups between the years 1999-2013 can be found here: http://wonder.cdc.gov/controller/datarequest/D76
The CDC also explores conditions that are often present when “disabilities” are present, what do these co-occurring conditions indicate in a holistic picture of health?
Studies have shown that individuals with disabilities are more likely than people without disabilities to report:
- Poorer overall health.
- Less access to adequate health care.
- Smoking and physical inactivity.
All individuals need preventative health care and health programs & interventions for the same reasons—to stay well, active, and a part of the community. Being healthy means the same thing for all of us—getting and staying well so we can lead full, active lives. That means having the tools and information to make healthy choices and knowing how to prevent illness. These correlated indicators, called: secondary conditions can include pain, depression, and a greater risk for certain illnesses.
Secondary Conditions
People with physical or mental conditions are often at greater risk for other health problems that can be prevented. Some of these other health conditions might include:
- Bowel or bladder problems
- Fatigue
- Injury
- Mental health and depression
- Overweight and obesity
- Pain
- Pressure sores or ulcers
http://www.cdc.gov/ncbddd/disabilityandhealth/relatedconditions.html
Issues regarding Bio-medical Ethics and Death and Dying
- Euthanasia
- Abortion
- Competency v Incompetency
- Quality v. Quantity of life
- Sanctity v. Salvation
- Death with dignity
Review this article/website and listen to the podcast. Review the resources on this website: https://cbhd.org/resources
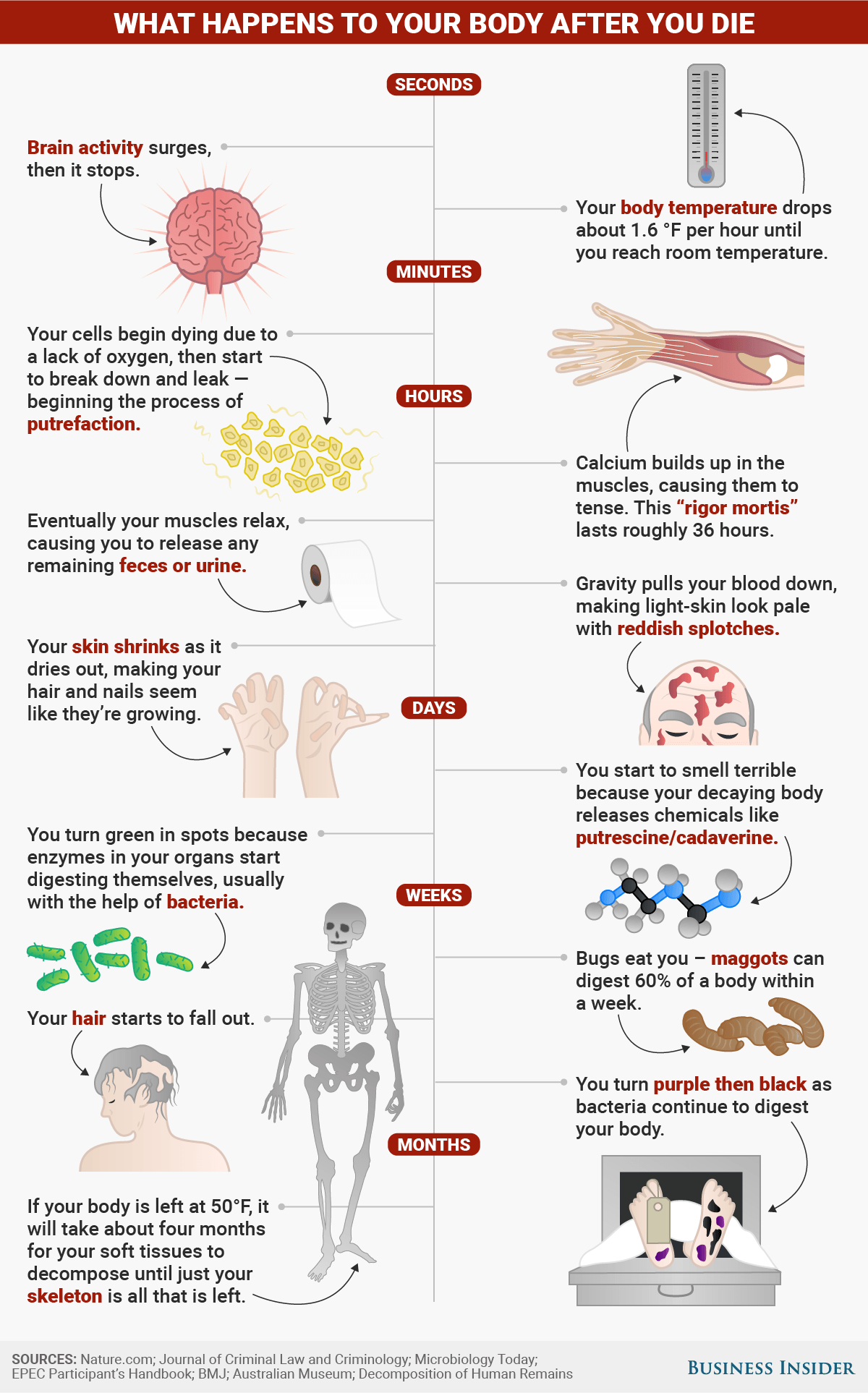
What happes to the body:
Assessment
Lesson 7 Activity
Examine ideas related to dying and death in health care settings, end-of-life ethics, dying as it relates to terminal or life-threatening illness and the concepts of grief and loss related. What is your opinion re: the two cases at the beginning of the lesson (Munoz & Schiavo)? Discuss your thoughts & feelings re: the cases, and then briefly take the opposite stance and present an argument for the ‘other side.’
Lesson 7 Discussion
The lesson resources estimated, at that time, that up to 5,000.00$/day for ‘health-care’ costs may accrue for patients for whom the definition of death becomes unclear. Assess health care practices with which you are familiar, and as mentioned in this lesson, based on your understanding of the biological and social factors that contribute to definitions of death/life present your view on health care practices for cases for which death/life can be debated. (You may want to look at Dying on Life Support: is it fair?)
Lesson 7 Quiz
- Define death, using your own words and the resources in this lesson.
- Define life, using your own words and the resources in this lesson.
- Give, at least three examples of health-care/death-care bioethical issues that may occur given the definition of death & life, along with the concepts discussed at the end of the lesson (death with dignity, competency v. incompetency, quality v quantity of life, for example.