Lesson 8: Neurocognitive Disorders and Alzheimer's Disease
Attention
Many people equate getting older with losing one's ability to remember things. This is actually a myth. There are individuals who experience neurocognitive disorders but this decline is not considered a normal part of aging.
Learning Outcomes
Upon completion of this lesson's material, students will be able to:
- MHRT Outcome: Understand interaction of co-occuring medical conditions
- Identify a medical condition that could result mild cognitive impairment or delirium
- Identify over-the-counter medications that might produce periods of mild cognitive impairment or delirium
- Reflect on the similarities between stigma associated with Alzheimer's and other minor neurocognitive disorders and stigma associated with other mental illnesses
- Analyze viewpoints on the traditional medical model of Alzheimer's and alternative views
- Locate available research on various causes of minor neurocognitive disorders aside from Alzheimer's Disease
Teaching
Intelligence
- Tends to remain stable throughout the life
- Late life terminal decline averaging 5 years before death
- Most likely associated with pre-clinical dementia
- Crystallized Intelligence vs. Fluid Intelligence (From Valliant Ch. 8, page 238)
- The more a skill requires Fluid Intelligence, the earlier it begins to decline
- Selective optimization and compensation (linked to functional skills)
Sensory Motor Functioning
- Changes in sensory motor functioning may impact testing for cognitive and intellectual ability
- Vision, hearing, touch, and motor function all may decline
Memory
- Episodic Memory
- Personal experiences in the world
- Changes in Episodic memory relate to specific brain lesions
- Semantic Memory
- Overall knowledge of the world, names of objects, etc.
- Temporal lobes
- Alzheimer disease effects semantic memory separately from episodic memory
- Procedural Memory
- Ability to learn behaviors and cognitive skills
- Procedural memory may remain intact even when episodic memory and semantic memory have declined
- Working Memory
- Also known as Short Term Memory
- Any disease, including Alzheimer and other dementias, that impact the frontal lobe will impact working memory
The concepts about memory are explained in more detail in these slides, please review: MHT216 Aging Memory Lesson FA16
Cognitive Impairment
Cognitive impairment is not the inevitable consequence of aging after maturity. The mind changes but most research has focused on cognitive deficits instead of cognitive growth.
- It is important to identify how well people function in their daily lives, not just objectively describe their cognitive abilities
- Many biopsychosocial factors impact the aging mind over the course of their lives (biology, psychology, social)
- The aging mind is adaptable and flexible
- Complaints regarding cognitive impairment may be due to situational factors (stress and anxiety), medications, or depression.
Please review the DSM 5 Neurocognitive Domains
These domains are important because each of these domains impacts the type and level of support an individual may need. These can used as part of your assessment of an individual's current functioning, current service needs and future service needs. There is a whole chapter in the DSM 5 about Neurocognitive Disorders. With the changes made within the DSM 5 it created a new classification system for cognitive impairments. If the cognitive impairments do not reach the threshold for a diagnosis of dementai they are termed mile neurocognitive disorders (NCD).
The diagnostic criteria within the DSM 5 for mild NCD include the following:
1) Evidence of modest cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual motor, or social cognition) based on: a) Concern of the individual, a knowledgeable informant (family member, friend or staff), or the clinician that there has been a mild decline in cognitive function; and b) A modest impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment.
2) The cognitive deficits do not interfere with capacity for independence in everyday activities (i.e., complex instrumental activities of daily living such as paying bills or managing medications are preserved, but greater effort, compensatory strategies, or accommodation may be required [from: http://www.jaapl.org/content/42/2/159.full].
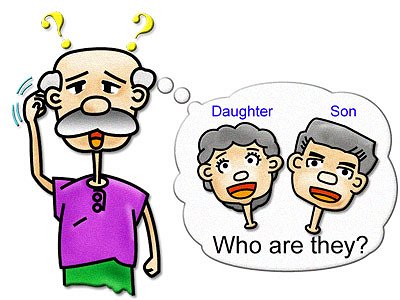
Mild NCDs live on a continuum from very mild symptoms to severe, labeled major, symptoms of NCD. So there are times when the distinction between major NCD and mild NCD can appear arbitrary so precise symptoms that distinguish mild from major are difficult to define. When we describe mild cognitive impairment it might look like the person is not presenting as their "normal" self. The client may be reporting complaints that they can't rember things or their family says, "My loved one doesn't seem like him/herself any more." About 40% to 80% of individuals who experience mild cognitive impairment go on to develop Alzheimer's Disease. Currently there are no effective treatments for mild cognitive impairments.
Dementia (The new term for dementia is neurocognitive decline)
- Defined as a loss of memory and other cognitive functions
- Criteria is outdated because we have a better handle on the early signs
- Alzheimer's/Dementia Resources in Maine
- Could be reversed if found to be associated with:
- Infections
- Nutrition
- Poisoning
- Cardiovascular and pulmonary disease
- Medications
- Visual or hearing loss
- Depression
- Isolation
Delirium
- Acute fluctuations in mental state
- Hyperactive, hypoactive, and mixed
- Inevitably associated with medical disorders and conditions
Alzheimer's Disease and other Dementias
Two major changes occurred in the DSM-5 related to Alzheimer's and Dementia. First, they have dropped the term "Dementia" in favor of "Major Neurocognitive Disorder". This changes occurred because of the stigmatizing use of the word "Dementia" and "Demented". This is very similar to when the authors of the DSM dropped the terms "Idiot", "Imbecile", and "Moron". All of which used to be clinical terms used to describe degrees of mental retardation. In the DSM-5 the term retardation has been removed and replaced with intellectual disabilities.
Another significant change is that the term “dementia” has been eliminated and replaced with major or minor neurocognitive disorder. It was believed that the word dementia was stigmatizing toward older individuals and not well accepted by younger individuals with HIV dementia. The new term focuses on the decline from a previous level of functioning as opposed to a deficit.
The old dementia terminology required the presence of memory impairment for all of the dementias. It has been recognized that memory impairment is not the first domain to be affected in all of the other diseases that cause a neurocognitive disorder. For instance, in frontal temporal disorder, language could be affected first. This change in terminology will require that all diagnosing healthcare professionals first establish the presence of a neurocognitive disorder and then determine whether the neurocognitive disorder is minor or major.
Read the rest of the article regarding the changes in the DSM-5 and their relations to cognitive disorders:
Dementia and DSM-5: Changes, Cost, and Confusion By James Siberski, MS, CMC
Click on the link below to visit the website of the Alzheimer's Disease International. Review the "World Alzheimer's Disease Report 2012 Executive Summary" and watch the video (both on the page when you click the link below. Very interesting information.
Alzheimer's Disease International Website
One of the most challenging aspects of this disease relates to how involved we try to make individuals in their own care (note in the video when the husband relates how important it is that people talk to his wife directly instead of always assuming they need to talk to him).
Issues of competence and ability to care for self are the pressing issues of Alzheimer's Disease patients and their families.
The subjective experience of Alzheimer's can be extremely frightening. Consider the "stages" that may present in the individuals experience the initial symptoms or diagnosis of Alzheimer's disease:
- Recognition and concern: "Something is wrong."
- Denial: "Not me"
- Anger, Guilt, and Sadness: "Why me?"
- Coping: "To go on, I must do..."
- Maturation: "Living each day until I die"
- Separation from self
Perhaps the one we hear about the most is the "Separation from self". Individuals whom I have encountered who have had loved ones with this disease talk about the "personality" dying way before the body does.
Similar to other "mental illnesses" Alzheimer's has a significant degree of stigma associated with it. As is discussed in the video, right at the time when these individuals need others the most, they are more likely to be alone.
There are, however, other viewpoints. I'm going to have you investigate an interesting perspective that I came across called "They Myth of Alzheimer's" Now, don't be alarmed, this is not a viewpoint that says that people are "faking it" or that the symptoms are not real, it is a critical analysis of the etiology of Alzheimer's, our reluctance to diagnose it (thus doctors are not telling the truth all the time), and findings that indicate that the physiological changes that happen in the brain (plaques) are not directly connected to the symptoms of memory loss and confusion.
You be the judge...
The Myth of Alzheimer's
Feel free to explore this website!
Check out this film: "The Diseased Other"
This lesson has you using an app called Mental Illness: Facts on Anxiety, Depression, Bipolar Disorder, etc. It lists a variety of mental illnesses and their defintions. It is a nice resource to have available to you to look up disorders like dementia but also other disorders we will be discussing in this course and your other MHT courses. Download the free app. Look up the definition of dementia. Review the list or search the list for other mental illnesses you are curious about. Mental Illness https://itunes.apple.com/us/app/mental-illness-facts-on-anxiety-depression-bipolar/id332173994?mt=8 - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - This app is called the Alzheimer's Association Caregiver Buddy. Think through if you were working with a client who was the caregiver for an individual with Alzheimer's disease. The caregiver might be struggling with doing activities and communicating with their loved one. Look through this app to find some suggestions for providing information to your client about things he or she could do to improve their interactions. The app is created and supported by the Greater Illinois Chapter of the Alzheimer's Association. I would expect the Live Help and 1-800 # resources would be connected to the services in Illinois. Alzheimer's Caregiver Buddy https://itunes.apple.com/us/app/alzheimers-caregiver-buddy/id994572444?mt=8 |
Assessment
Lesson 8 Discussion (online course only)
Explain how you might feel when you encounter clients who may be experiencing mild, moderate or major neurocognitive decline or a diagnosis of Alzheimer's Disease. If you have personal experience you can share those experiences as well. Clients presenting with neurocognitive decline can be very challenging because they may lack short term memory, present with agitation or extreme emotions of anger or sadness.
Lesson 8 Quiz
- Research a medical condition online that could result mild cognitive impairment or delirium. Please indicate what the name of the medical condition, what it is, and what the symptoms look like. What might the cognitive impairment look like if you were meeting with this client?
- Go to a drug store or grocery store. Locate a medication that is sold over the counter. Look up the side effect details on the packaging to see the possible cognitive side effects of the medication. List the mediction you selected, what it is used to treat and summarize the cognitive side effects you found.


